
An international team that includes researchers John Spencer, Ph.D., and Charlotte Avanzi, Ph.D., of the Colorado State University Mycobacteria Research Laboratories has identified leprosy in wild chimpanzees in the West African countries of Guinea-Bissau and Ivory Coast.
In a related study published in Nature, the team describes how leprosy had never been documented in wild chimpanzees. The authors say that the bacterial strains were different in both countries and very rare in humans.
The finding could indicate an unknown source of leprosy in the wild and reveal new clues about a still-mysterious disease.

Avanzi and Spencer spoke with SOURCE about this latest research and their ongoing studies on leprosy.
Q: How difficult is it to study leprosy?
Avanzi: The difficulty of studying leprosy adds to the lack of interest. The bacteria that cause the disease, called Mycobacterium leprae, cannot be cultured in the lab. The only way to multiply the bacterium is in animal models such as armadillos or into the footpads of mice. These experiments are very difficult to execute and there is only a handful of laboratories in the world with this expertise. That is why our group studies the bacteria directly from an infected person.
We are more specifically interested in looking at the genetic differences of the bacterium infecting different individuals. However, there is only a tiny number of bacteria in each sample, so our group has developed several tools that allow us to recover as much bacterial DNA as possible from these precious samples.
Q: How did you become involved in this research, after the discovery was made by conservation scientist Kimberley Hockings about the chimpanzees?
Avanzi: I did my doctoral studies in Lausanne, Switzerland. Before I came to CSU to start my postdoctoral work in Professor Jackson’s laboratory, I was contacted by a team in Germany working with Kim [the first author of the study] studying chimps in Cote D’Ivoire. They had isolated bacterial DNA from the chimps’ feces that was shown to be M. leprae but they needed our tools to obtain the full genome. In December 2018, using a new approach, I was able to run additional experiments in Lausanne to get the whole genome sequence data that I analyzed at CSU. In addition, they needed help to show a positive antibody test for leprosy in infected chimpanzee serum.
Spencer: We had some rapid serological tests that we used for this research. They were developed for human leprosy cases and are up to 95% positive in human lepromatous leprosy patients. It’s a very sensitive test. These tests confirmed the leprosy findings in the wild chimpanzees.
The fact that chimps are very closely related to humans helped, since the antibody response to the antigen would be easily recognizable.
Q: How could these strains be that rare in humans and exist in another environment or reservoir?

Avanzi: The bacterial strain identified in chimps in Côte d’Ivoire is related to modern strains found in patients in Ethiopia and to ancient strains that were circulating in medieval Europe. There are different hypotheses that could explain its origin. It might be an old infection where the bacterium was circulating in humans and introduced in the chimpanzee population and transmitted inside the community over time. However, we haven’t done much research on villages or cities around these parks so it could also be that the strain is still present in humans in these particular areas and was recently transmitted to animals.
Another hypothesis would be that the bacterium survives in an environmental or other animal reservoir in the park and was transmitted to the chimpanzee recently or in the past. The bacteria cannot live outside a host but can survive and persist in amoebae or insects in laboratory settings. Maybe such a reservoir also exists in the wild, but we haven’t found it yet.
Q: What other leprosy research would you say has been significant in your career?
Avanzi: In 2016, we also reported leprosy infection in red squirrels in the British Isles. This study really changed our knowledge about the disease since it was the first time that leprosy was found in a wild animal reservoir in Europe. Before that, the only reservoir was wild armadillos in the southern United States..
It had been previously shown that captive chimpanzees in zoos could become infected with leprosy, probably getting it from their human handlers. With this latest discovery of leprosy infecting wild chimpanzees in Africa living completely isolated from humans in national parks, it becomes more likely that it came from an environmental source. This represents a unique opportunity to further study how leprosy can be transmitted in animals and humans from a potential reservoir that we just don’t know about yet.
Spencer: In most cases, it’s been assumed that humans must transmit leprosy to animals like armadillos in the US or red squirrels in the UK. There had to be an event where humans transmitted bacteria first to animals.

With armadillos, there could be spillback to humans. That was what we discovered in Brazil in 2018. We found compelling evidence that the armadillos could transmit the bacterium to humans.
Dr. Richard Truman at the National Hansen’s Disease Program (NHDP) in Baton Rouge, Louisiana, essentially identified one specific genome in most armadillos that is identical to the ones which were found in humans in the southern US. That’s been well documented. There’s a second genotype that occurs in a cluster of leprosy cases in armadillos and humans in Florida. These unique strains are found in both armadillos and humans indicating a zoonotic infection in armadillos that is then passed back to humans.
Q: What are the next research steps to study leprosy transmission?
Spencer: Leprosy had been a human disease for thousands of years before discovering all these animal reservoirs. It’s not an emerging disease yet it is the oldest known disease associated with humans. It’s also unlikely that it will disappear soon. We really need to figure out how to approach this disease differently to eliminate it from humans at some point.
In the US, armadillos are increasing their range. They came up from Mexico in the 1850s and spread from Texas across the southern states. And then there was a separate population that escaped from a zoo in Florida. These two populations eventually merged. In areas where armadillos aren’t as common, like Georgia, they’ve documented cases of leprosy in people. These are rare instances but it’s plausible that the infectious source or bacteria can survive in the ground.
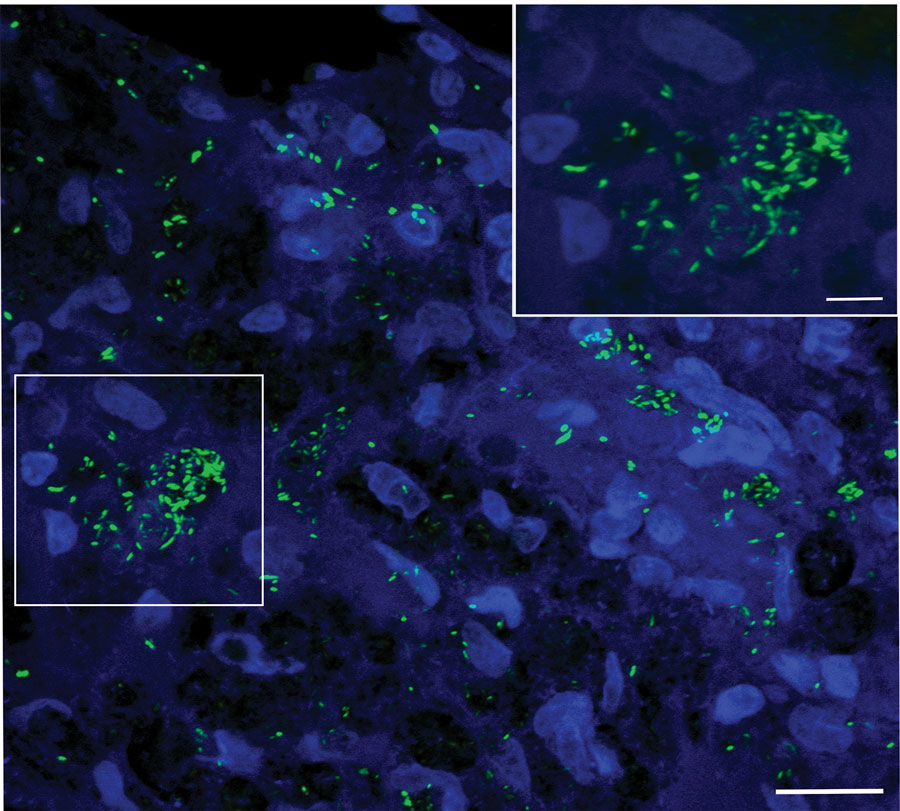
We recently published a Research Letter in the Journal of Emerging Infectious Diseases about a wild armadillo infected by M. leprae in the state of Nuevo León, Mexico. Nine-banded armadillos (Dasypus novemcinctus) are naturally infected with Mycobacterium leprae (pictured below) and are implicated in the zoonotic transmission of leprosy in the United States. In Mexico, the existence of such a reservoir remains to be characterized.
Avanzi: In leprosy, it had been assumed that transmission between humans was the main source of infection. In the last few years, the work on animal reservoirs has pointed the research towards a transmission line that also include animal. The study in Africa also raises the possibility of an environmental reservoir. The team in the UK is working on a follow-up study with the chimps in Guinea Bissau.
This time, they will include human and animal health policies and include environmental screening. This is called a One Health approach in which the health of people is considered closely connected to the health of animals and the shared environment. They want to help educate people in the villages about how to approach any animals if found dead, and hope to create a national education program about the spread of disease. Education and avoidance can prevent transmission. Future work should focus on a similar One Health approach in all leprosy-endemic countries.
Mary Guiden conducted this interview, which was edited for length and clarity.