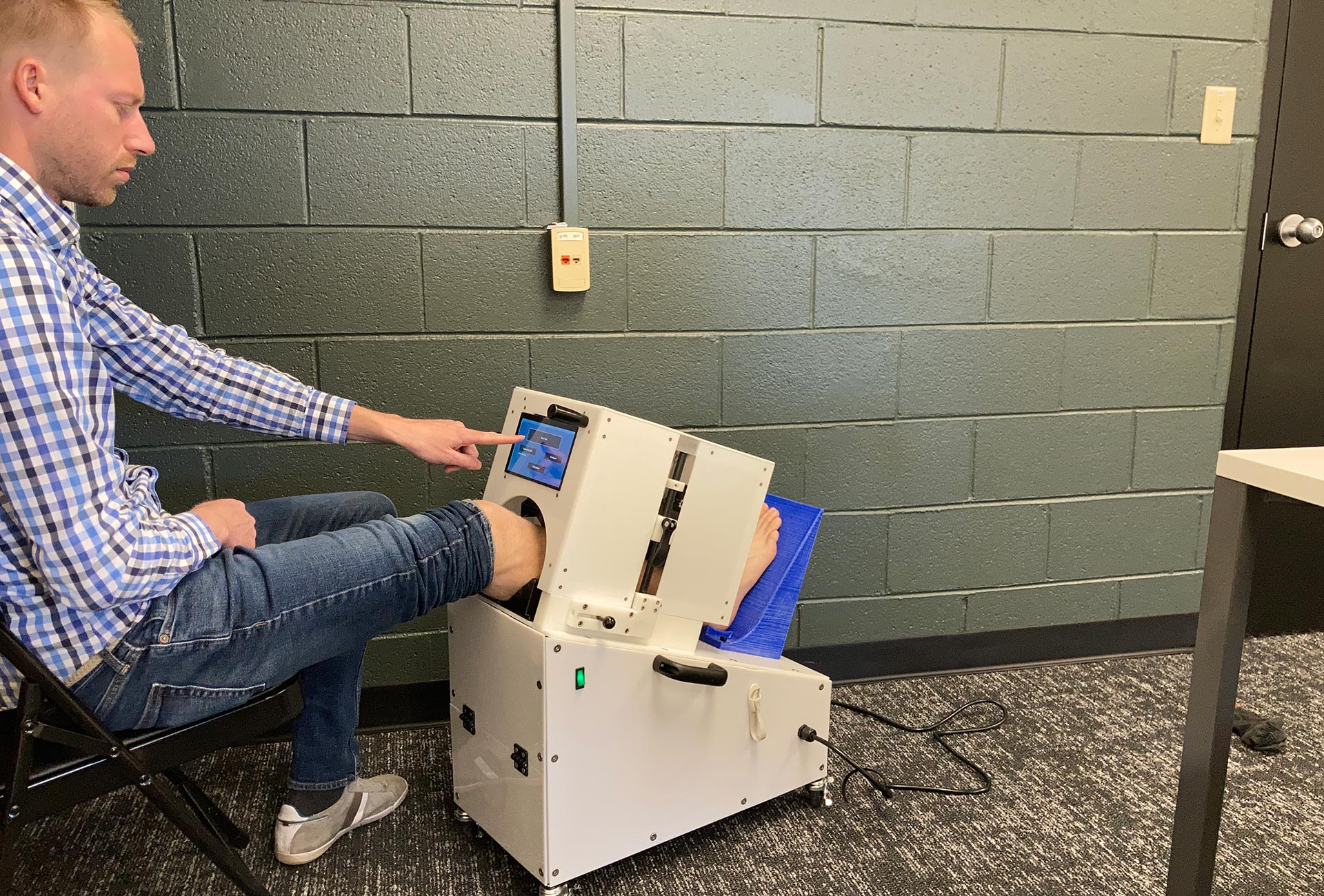
CSU research scientist Kevin Labus demonstrates the tibia fracture device, now being used in a study with UC Health patients.
Fracturing one’s tibia, or shin bone, is a common orthopedic injury. It’s a severely disruptive injury for anyone, but it’s especially traumatic for the unlucky few whose fractures don’t heal the way they’re supposed to.
People who fracture their tibia usually get hardware surgically implanted to hold the bone in place. After about six months, 10% of patients are diagnosed with what’s called a non-union fracture, or a failure to heal; they require additional surgery to implant new hardware, and the waiting, pain and discomfort – not to mention the financial burden of another surgery – starts anew.
The standard method to diagnose a non-union fracture is through X-ray, but X-rays cannot capture the subtle mechanical details of how well bone tissue is mineralizing and stiffening soon after the injury. What if there was a way this stiffening could be detected much earlier than six months post-injury, so doctors could intervene faster?
Nearly two decades ago, Colorado State University biomedical researcher Christian Puttlitz, then early in his career as an assistant professor at the University of California San Francisco, first put his mind to this question, wondering whether innovations in engineering and biomechanics could provide insight into the healing potential of bone. From that inspiration sparked a series of experiments that led to a present partnership with UC Health doctors and patients, who are currently helping test a fracture-detection device Puttlitz and his lab have been working on for the last several years.

‘Holy grail’ for orthopedics
“Trying to figure out what’s going on at a fracture site has been described to me by many people as the holy grail for orthopedics,” said Puttlitz, who heads the Department of Mechanical Engineering at CSU, teaches in the School of Biomedical Engineering, and runs the Orthopaedic Bioengineering Research Laboratory. “If you could figure this out, it would make a huge impact on the practice of fracture management.”
Over the last year, Puttlitz and CSU research scientist Kevin Labus have been partnering with UC Health on a groundbreaking study funded by the National Institutes of Health to gather data on patients with tibia fractures. With the help of UC Health trauma surgeons, the researchers are testing their device with 16 volunteer patients, who are using the device once a day in their homes and providing data to the research team.
The device consists of an enclosure that applies gentle, non-painful pressure on the patient’s fracture site. An external radio antenna sensor measures deflection under loading, and the sensor is calibrated to measure bending stiffness of the fracture callus. Down to 10-micron precision – with much more accuracy and detail than an X-ray – the device lets the researchers assign a value to how well the bone is stiffening – an indication of normal healing – starting about six weeks after the initial injury. That’s much sooner than the six-month mark patients usually have to wait to find out whether their fracture is mending properly.
Switching from chip to antenna
The device is the result of many years of iteration, stops and starts. When Puttlitz first envisioned the device, it was built around a chip that, when implanted on top of the patient’s fixation hardware, would read out the bending stiffness of the injury site through electromagnetic resonance. This design went through several rounds of inquiry, including animal studies and production of data that proved out the concept, but the chip introduced challenges from environmental interference. Also, an implantable chip is invasive and would require rigorous FDA approvals for an eventual clinical trial.
When Labus joined the project in 2016, the chip idea was replaced by the external antenna that would electromagnetically couple directly to the patient’s rod or plate hardware. Led by Labus, the group began collecting data showing the antenna-based design worked as well or better than the chip, with more accurate readouts. The new, external antenna method also allowed the team to start testing fracture patients without regulatory hurdles, since it did not require invasive procedures.
They also teamed with electrical engineering Professor Branislav Notaros, whose group performed computational simulations to validate Labus’ data and also designed a smaller, flatter antenna that allowed the team to create an array of sensors for much more precise measurement.
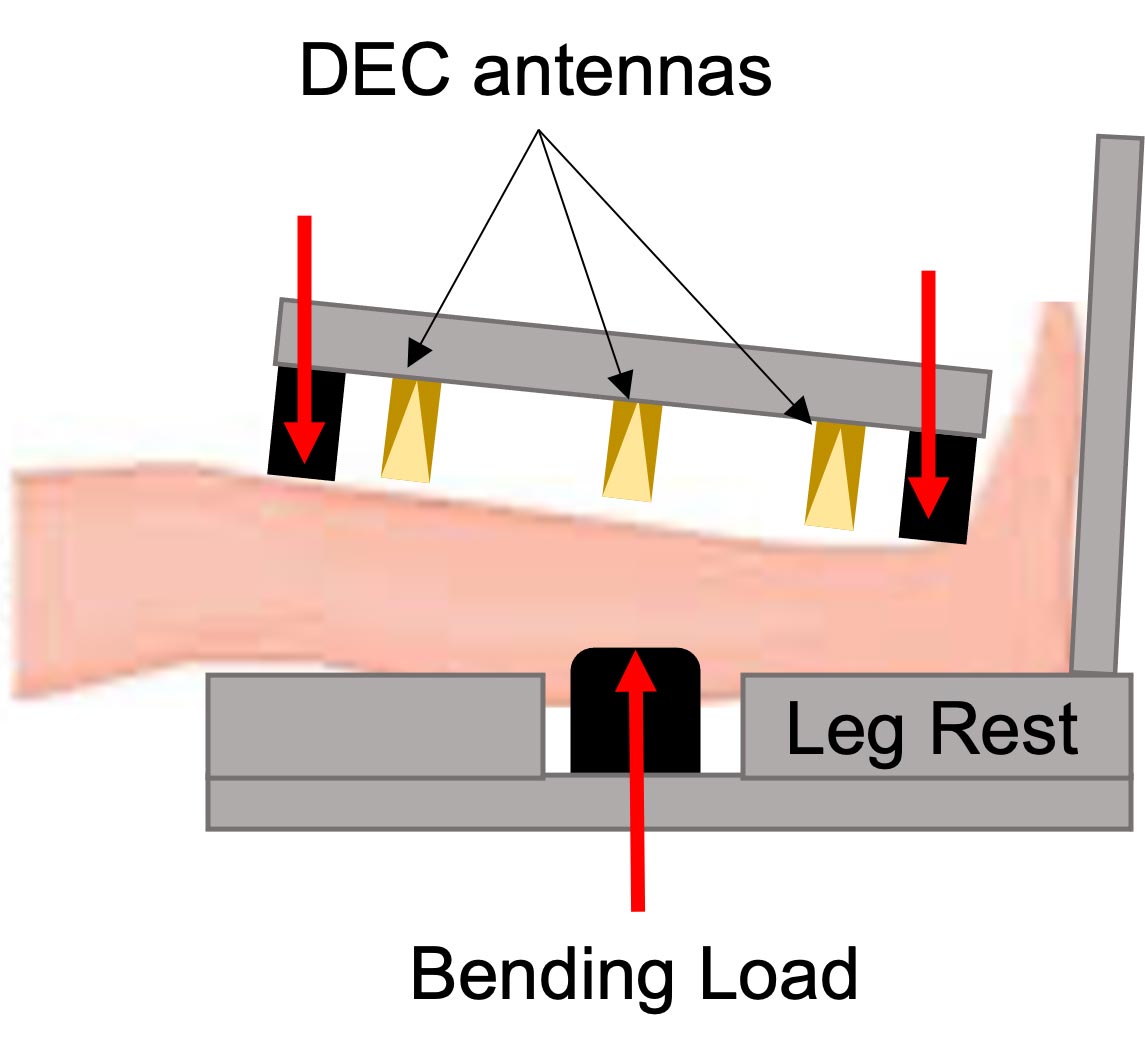
A schematic that shows how the fracture detection device’s current design works on a patient.
Future directions
Labus’ current UC Health study is testing the feasibility of the device as a healing indicator; no data is being shared with patients or doctors. The eventual goal is to provide such information to doctors so they can identify and correct non-union fractures earlier than six months post-injury.
There’s lots more work to be done. The next step will be a larger observational study followed by a clinical trial, using the bending stiffness data to identify patients at risk of non-union diagnosis and to guide early interventions for improving healing. Years of hard work have led the team to this moment, and they’re actively seeking additional partnerships to continue proving out their device.
“This combination of applying engineering to solving medical problems is what excites me the most,” Labus said.