By Sarah Ryan
When Dr. Gregg Dean first saw the genomic sequence of SARS-CoV-2, the virus that causes COVID-19, he recognized an old foe. It was early January 2020, more than two months before the World Health Organization would declare COVID-19 a pandemic. Dean had studied feline coronavirus since the ’90s, and the similarities between the two diseases were striking.
“The silent shedders, the possibility for reinfection, the short durability of the immune response, the disparity in individual outcomes, and the way the disease attacks a lot of organ systems,” Dean says. “These findings are all reminiscent of what we’ve always observed in cats.”
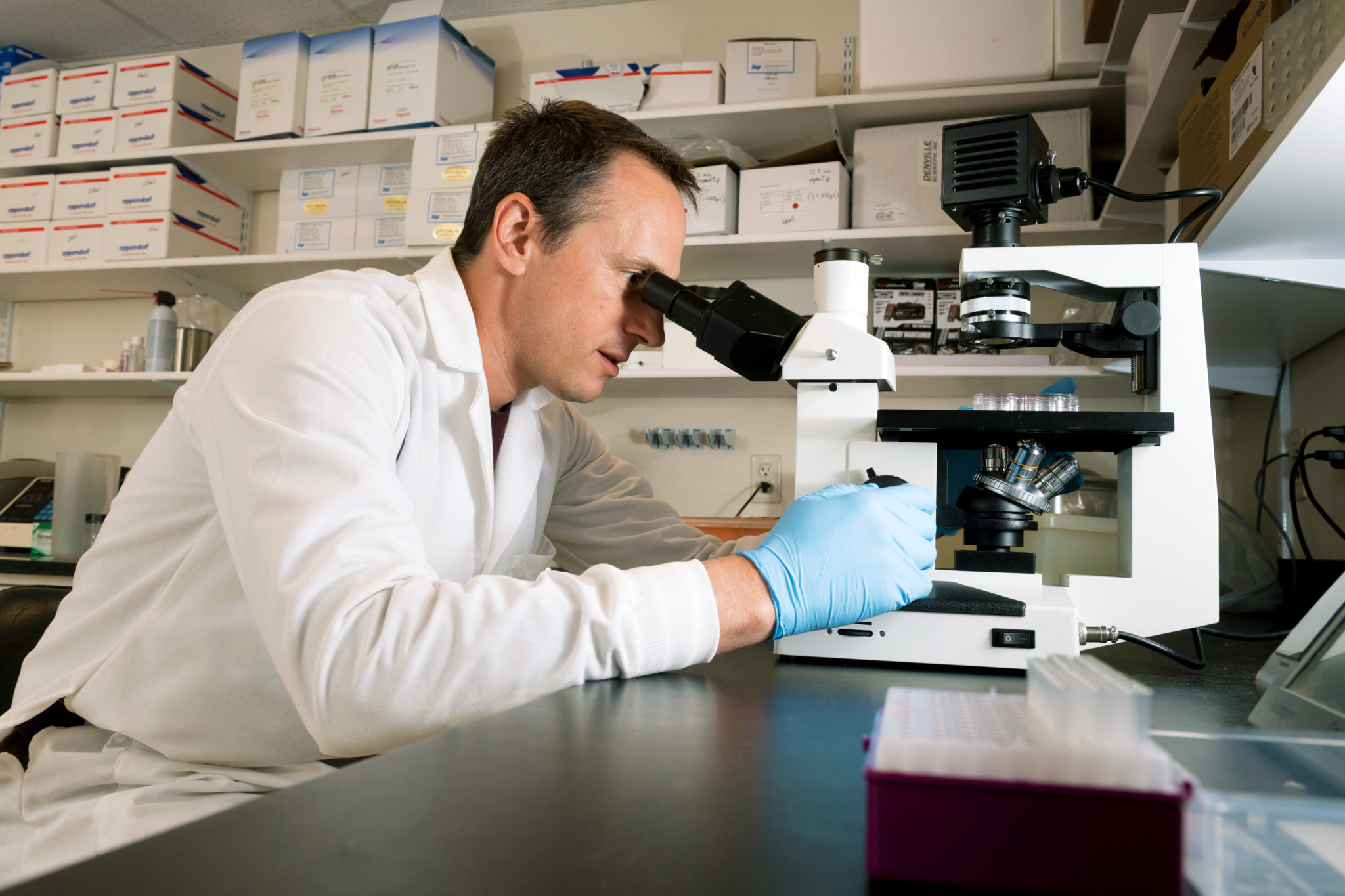
Dean is an immunologist and veterinarian who has worked on many vaccines, including a feline coronavirus vaccine for the Morris Animal Foundation. “We had dwelled on the feline virus for so long, just looking at it, trying to contemplate where do you hit this thing? Where is the soft spot in this virus? There are a couple places that are critical to its ability to infect, to replicate, and to be transmitted,” Dean says.
His vaccine strategy was the first to target those “soft spots.” His team recognized the same targets in SARS-CoV-2 and began to work on a human vaccine strategy in early 2020.
This is an ideal example of academia in action during a crisis, but it is by no means an isolated incident in the College of Veterinary Medicine and Biomedical Sciences. Researchers from across the College responded immediately to the pandemic, pivoting overnight to COVID-19 vaccine development, antiviral therapies, testing, and diagnostics. By April 2021, CVMBS scientists had submitted 183 proposals and received $31 million in funding for COVID-19 research.
The pandemic is far from over, yet the past year contains ample proof that the College will help end it. We spoke to faculty, staff, and students who have contributed to this massive effort, and from their stories we distilled the 10 practices that make us pandemic-proof.
Invest in collaborative people...
When Candace Mathiason became the director of the Infectious Diseases Research and Response Network, her primary goal was to connect people across disciplines.
“We joked about how it’s like Tumblr for scientists. Swipe right if you have a connection,” says Mark Zabel, associate dean for research. “Dr. Mathiason’s vision was to seek out expertise, understand our strengths, and then start putting people together.”
Mathiason hosted biannual pitch events, where IDRRN researchers could pitch ideas and then form affinity groups. “That was a great idea that really hit its stride when the pandemic started,” Zabel says.
On March 17, 2020, Mathiason assembled a roomful of virologists, immunologists, evolutionary biologists, microbiologists, epidemiologists, and veterinarians and asked what they could do about the pandemic. They discussed diagnostics, surveillance, PPE, and vaccine strategies, among other things.
As the ideas began to cross-pollinate, Mathiason focused on connecting researchers and identifying funding sources.
“The collaborative component was so easy because people were so willing to step forward and do this work,” Mathiason recalls. “They had an altruistic need to be a part of the answers. This is what we’ve been training for most of our careers. When we saw it happening, we thought, here it is. I can have an impact. I can make a difference.”
... and pioneering facilities and technologies
At the pandemic response meeting, virologist Rushika Perera volunteered to test antiviral therapies. Antivirals are drugs, compounds, and chemicals that might be used to treat individuals who have contracted COVID-19. The Centers for Disease Control and Prevention requires that SARS-CoV-2 experiments occur in Biosafety Level 3 laboratories. There are only 14 regional biocontainment facilities in the United States, and one of them is at CSU. One week later, Perera had established a Respiratory Virus Wing within the BSL-3 facility and begun testing hundreds of antivirals from local, regional, national, and international groups, including academic collaborators and private companies and organizations.
At the same time, virologist Greg Ebel, Sc.D., was increasingly concerned about the lack of COVID-19 testing among health care workers. “At that point, we really didn’t know when somebody could be infectious. We needed to test health care workers to protect the health care system from collapsing,” Ebel says.
The RNA extraction robot he used to study West Nile and Zika viruses would work just as well on SARS-CoV-2. Ebel teamed up with Dr. Nicole Ehrhart, director of the Columbine Health Systems Center for Healthy Aging, and they began testing asymptomatic health care workers in long-term care communities.
Ebel and Ehrhart created a surveillance program, but they needed high-throughput genomic sequencing to turn thousands of samples into useful bioinformatics. They turned to Mark Stenglein, director of CSU’s Next Generation Sequencing Core.
“At a global level, scientists have been sequencing the genome of SARS-CoV-2 in a way that is completely unprecedented in the history of pandemics,” Stenglein says. “The goal of all that genomic sequencing is to understand how the virus is spreading around the world. We can look at really local chains of transmission, like in a long-term care facility, and global patterns, like timing, directionality, and movement of the virus, and how it’s mutating to become more or less infectious.”
That’s big data, and Stenglein’s team needs powerful servers, specialized software, and dedicated facilities to generate and analyze it.
In October 2020, many of the researchers studying COVID-19 moved into a new research facility called the Center for Vector-Borne Infectious Diseases. The 41,000-square-foot facility was three years in the making, but its completion couldn’t have been timelier. The open-concept labs bring to life the collaborative, interactive approach necessitated by the pandemic.
Fight every infectious disease.
Pre-pandemic, Dean was attempting to develop a feline coronavirus vaccine based on the probiotic lactobacillus acidophilus platform.
Ray Goodrich, Ph.D., director of the Infectious Disease Research Center, and Dr. Dick Bowen, professor of biomedical sciences, were developing vaccines for African swine fever using a blood safety technology called SolaVAX™.
For 25 years, geneticist Mary Jackson, Ph.D., has studied tuberculosis, which was the deadliest infectious disease in the world before COVID-19. Now, Jackson is attempting to develop a COVID-19 vaccine based on the Bacillus Calmette-Guérin vaccine for TB.
Veterinary pathologist Amy MacNeill is an expert in poxviruses. She was attempting to create an anticancer vaccine based on a poxvirus platform, and now she’s using that platform to target SARS-CoV-2.
That’s four different vaccine platforms for four distinct diseases that are largely – with the exception of cancer – regarded with apathy in the United States. Now, these research programs could yield vaccines that will be essential in the long-term fight against an evolving coronavirus. These second-line vaccines can be delivered to low- and middle-income populations where cost or infrastructure prohibit the use of vaccines based on an mRNA platform. They may also target the virus as it evolves.
“When we get a vaccine out there that looks like it’s working, we will find out about its weaknesses, so we will have a second generation, and a third generation, and a fourth generation of vaccines. It’s an important evolution of our prevention strategies,” Dean says.


Celebrate dead ends.
“If you work in vaccines, you realize that most vaccine candidates fail,” says Dean, who has also researched vaccines for rotavirus and HIV. “We’ve poured a lot of effort into HIV, and we still don’t have a vaccine, so the rate of failure has been 100%. It’s a little daunting to jump into a field where you know the chances of success are extremely low. But it doesn’t mean you don’t keep trying, and you learn from what has been done before.”
Our research teams persist despite the possibility of failure. Zabel emphasizes that every effort is valuable. “What not to do is just as important as what to do. If a vaccine or a therapy doesn’t work, that tells us something. It adds to the data, and that’s important.”
Think like an ecologist.
Virus strains similar to SARS-CoV-2 have been found in horseshoe bats, which are abundant in Asia. The coronaviruses that cause SARS and MERS also, most likely, originated in bats. Bats are essential to understanding the evolution and movement of zoonoses – diseases that originate in animals and then transmit to humans – so it’s a good thing that virologist Rebekah Kading, Ph.D., loves bats.
“They’re really fascinating creatures, and they provide so many ecological services. They are important for pollination and seed dispersal and insect consumption. There’s just so much to learn and appreciate about bats,” Kading says. Kading studies wildlife species, emerging pathogens, and spillover – the movement of a virus from a reservoir host into a new species – and that requires thinking like an ecologist. “I look at the interactions between people and wildlife, and ask ‘what are the risk factors that cause a virus to jump from one species to the next?’”
As soon as the pandemic permits, Kading’s team will travel to Uganda to study bat populations. “We’re looking at the ecology of the bats, seasonal patterns of virus shedding, and the human interface. What behaviors put people at risk as far as entering caves or handling the bats?” They will also watch for spillback – the potential for the SARS- CoV-2 virus to move from humans into the bat population.

Kading calls the COVID-19 outbreak “unprecedented” because there are so many ecological and biological barriers to spill-over. Immunologist Tony Schountz, Ph.D., agrees. “In the wild, most of these viruses circulate without causing substantial disease, because if they did, they’d kill the animals and lose their homes, or the animal’s immune response would clear the infection. These viruses have to behave like Goldilocks, right? They’ve evolved with a certain set of constraints that have been imposed upon them by their reservoir host’s genetics and biology. Then they get into another animal like a human, and suddenly those rules are no longer applicable.”
Coronaviruses “terrify” Schountz, but he is quick to point out that although three zoonotic coronaviruses have emerged in two decades, it’s not because the viruses have made an evolutionary leap. “It’s human behavior. Human encroachment on habitat. Increased population densities. Highly mobile societies and developing economies. And so these statistically unlikely events become more and more likely.”
Dream big.
SARS-CoV-2 spillback has already occurred in the United States in captive and wild mink populations, and Schountz and colleagues have demonstrated that deer mice and other rodents are susceptible to the virus.
“This virus could get permanently established, and that means it’s going to be a perpetual threat,” Schountz says. As the virus adapts to new hosts, genetic mutations could render front-line vaccines obsolete, which is one of the reasons that Dean, Ebel, Bowen, and other colleagues are beginning to work on a pan-coronavirus vaccine.
“There are a lot of coronaviruses out there, so this vaccine would confer protection against stuff we know about, but also things that we don’t know about,” Ebel says. “The idea is that this is probably going to happen again at some point, so we’d like to be prepared.”
It’s an ambitious project, and it will require a highly collaborative team of virologists, immunologists, microbiologists, geneticists, computational biologists, and veterinary pathologists. “I think it is truly remarkable to consider how many different ways we are bringing our expertise to bear on this problem,” Dean says. “It speaks to how robust this College is, the diversity of the expertise that we have, and the absolute commitment and passion to have an impact and to rally when society has a health care need.”

Tear down the ivory tower.
Lifesaving discoveries sometimes get stuck in the pipeline, or the freezer. Rift Valley fever, for example, is an emergent pathogen with the potential to devastate agriculture. The Centers for Disease Control developed a vaccine candidate, but the vaccine sat in a freezer for a decade because they lacked a manufacturing partner. Then John Wykcoff, director of BioMARC, got involved. BioMARC is a CSU nonprofit that partners with companies and government agencies to commercialize and manufacture drugs and vaccines for high-consequence pathogens. Now, CSU is partnering with the CDC and UC-Davis to bring the vaccine to the market.
BioMARC is one pillar of the Infectious Disease Research Center. The center also depends on the Regional Biocontainment Lab and the Research Innovation Center to defeat global health threats. Director Goodrich says innovation is at the heart of IDRC. “Innovation is not just invention,” Goodrich says. “It’s about finding ways to translate discoveries into practical solutions to the problems that vex our community.”
At the Infectious Disease Research Center, faculty labs are located in the same space as private companies working on a wide variety of products, from cancer treatments to flu vaccines.
“These private companies benefit by being able to collaborate with our faculty and students and utilize our resources. We’re establishing communication paths and networks that allow the exchange of ideas and information,” Goodrich says. “But if people are discovering and inventing new drugs, new diagnostics, new therapeutics, there’s still a gap between those ideas in the lab and making products that people can buy. BioMARC was established to bridge that gap, to take initial concepts that people have about how to solve a problem in the infectious disease space and translate them into processes and products.”
The National Institutes of Health has already funded $26 million for COVID-19 vaccine research at the Infectious Disease Research Center. CSU may be the only institution in the United States where every stage of vaccine development (with the exception of human trials) and manufacturing can occur in one place.
Train the next generation of scientists.
Kim Shelton first dreamed of a research career in the seventh grade, when she visited CSU’s microbiology department during the state science fair competition. As a CVMBS undergraduate, she began working in Dr. Dean’s lab on the probiotic vaccine platform. When the lab pivoted to COVID-19 vaccine development, Shelton worked alongside professor Allison Vilander on the vaccine construct.
“It was just the two of us at the start of the shutdown. We were taking the genes of interest for the proteins from the virus and getting them into the bacteria and getting them expressed on the surface,” Shelton says. “It would be really rewarding if a vaccine that I was able to help within its very early stages actually made it to the public sphere.”
Student researchers have played an essential role across the breadth of CSU’s COVID-19 response, from testing therapeutics to developing the campus surveillance program. Every researcher we interviewed for this article highlighted the role of undergraduate and graduate students in their research programs.
Mathiason emphasizes that training the next generation of scientists begins with K-12 STEAM programming. “We have to reach into K-12 and start planting the seeds that anybody who’s interested can be a scientist. You don’t have to have special skills to be a scientist. It’s just curiosity and wonder and an interest in what’s going on around you in the world. That’s all the starting materials that you need to become a good scientist.” Mathiason co-founded the Women in Science Network to foster inclusivity in science. WiSCI’s programs – including career issue groups, a lecture series, and an annual symposium – utilize conversation and community to build a multitiered and multi-generational mentoring system for scientists at every stage of their careers.

Attack the infodemic.
Research is a lighthouse in the storm of misinformation.
“Despite the politization of science and vaccines, science will save us and get us back to school and work,” says Kristen Browning-Blas, director of communications for the College. “Telling the story of science – what it is and how it touches your life – has felt more urgent than ever before.”
As Colorado went into lockdown, faculty and staff teamed up on internal and external communications. Ad hoc emergency response teams tackled the logistics of how to safely keep the veterinary hospital and other clinical services open and essential research and diagnostic facilities functioning, while public health guidelines changed daily. At the same time, Browning-Blas’ team focused on sharing stories of our research with the public. As COVID-19 fatigue set in, they launched a biographical video series called Staying Human.
“It felt like we were writing the first draft of history, and I’m really interested in how people are coping through this experience,” Browning-Blas says. “Staying Human was an opportunity to show that scientists are human too.”
Prepare for disease X.
“Outbreaks are inevitable. Epidemics are optional.” – Dr. Larry Brilliant
The World Health Organization maintains a list of priority diseases that pose the greatest public health risk due to their epidemic potential or the current lack of countermeasures. The current list begins with COVID-19 and ends with “Disease X.” Disease X represents the pathogen we don’t know about – yet.
“We have big problems on Earth right now with land use changes and environmental disruption. We’ve gotten really good at moving ourselves and our stuff around the world, and that’s driving this drumbeat of virus emergence,” says Dr. Ebel. “That’s why I’m interested in disease surveillance and virus evolution, but it’s not going to be me sitting in my lab that solves the problem. It’s going to be groups of people who can work at multiple scales and across multiple disciplines.”
In other words, one coronavirus vaccine – or a dozen – will not solve the global threat of emerging diseases. For the majority of priority diseases, there are no vaccines and few treatments. Combine that lack with the triple threat of globalization, urbanization, and climate change, and the next epidemic is inevitable.
Or is it?
If we change how we think about and prepare for infectious diseases. If we prioritize all diseases regardless of the communities they affect. If we work globally across borders, economies, and disciplines. If we learn from COVID-19, then the next pandemic is not inevitable.
Want to support our researchers? Click here to give!